Sarah Butcher: Tell us about your job title, and what your job entailed before the quarantine / pandemic?
Christine Chester: I have been a Medical Social Worker since 2013. I have worked in various units, NICU, L+D, Ortho, ICU, Med-Surg, Oncology, Trauma, Peds, Psych Evaluations, and the list goes on, always in acute care settings. At this time, I am the Medical Social Worker in an Emergency Department. As usual, the first and most valuable intervention is a thorough biopsychosocial-spiritual assessment. Once that is complete, I move on to facilitate my portion of the care plan as directed by the physician. Generally patient needs that are referred to me are centered around homelessness, abuse, poverty and lack of resources and safety concerns.
Sarah: How has the environment at work changed since the pandemic?
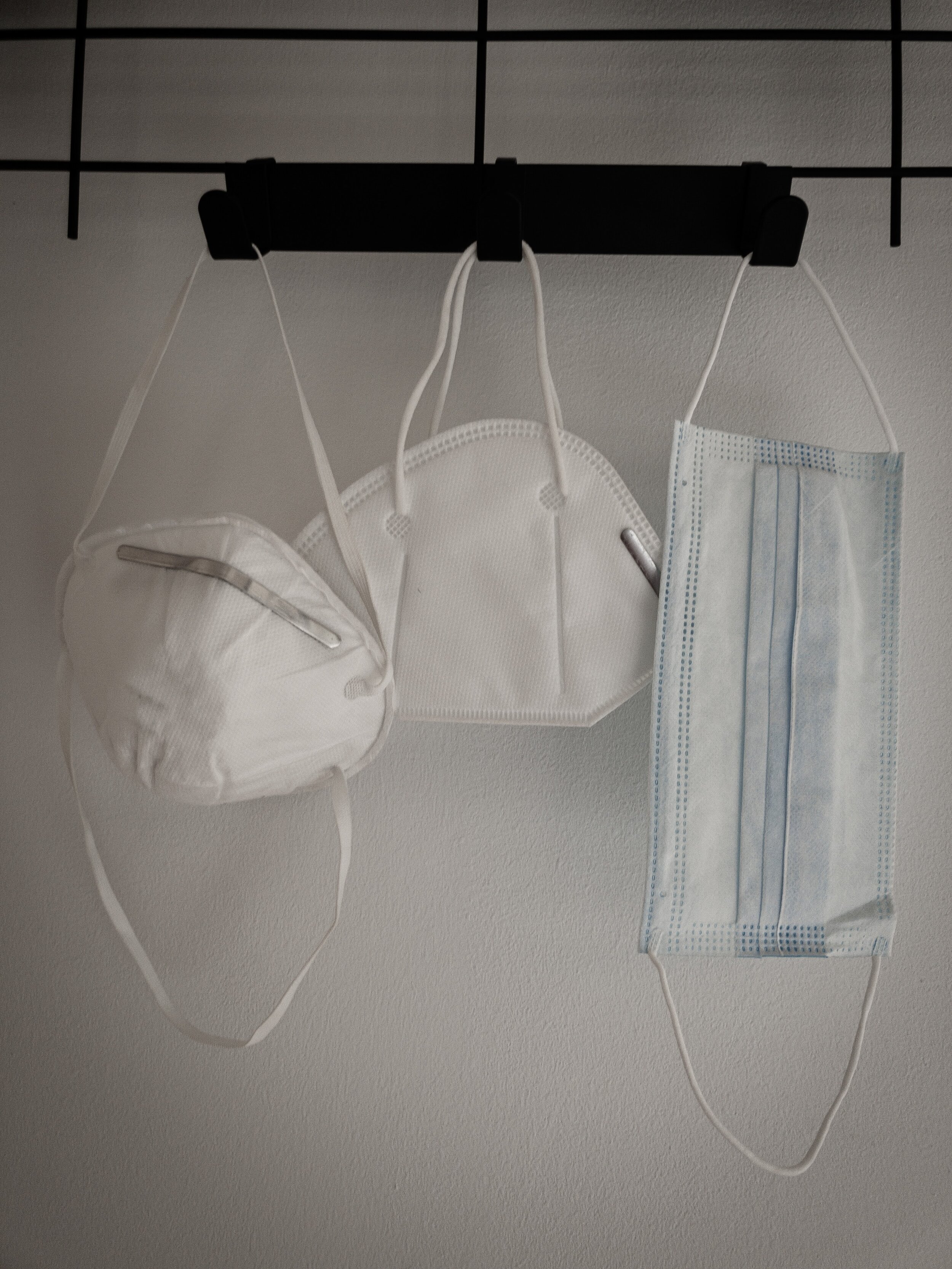
Christine: It’s very different. Simple things take much longer because of new processes. Wearing an N95 can make it more difficult to communicate, even over the phone. Even a simple mask can cause some skin breakdown or burdensome tension headache. It’s mentally taxing to consider a pathogen throughout the day, sanitizing and sequencing movement just to get a drink of water or use the bathroom.
We don’t have the typical mix of patient needs that we used to see--instead we are seeing many more critically ill patients. It’s truly unprecedented. I’m located in the nurses’ station. I try to prioritize patients who have a poor prognosis, and I complete those assessments first. As usual, I am inquiring about legal decision making, but often I’m having more expanded conversations about a POLST or an Advance Directive. I’m also trying to be sensitive to the needs of patients who are unstable. If a patient may not survive and they are transported to ICU, I try to communicate with the medical team about how and when to facilitate a video call. My goal is for loved ones to have as much connection as possible with their loved one. Sadly, that can mean facilitating a goodbye call, or comforting a visitor who is permitted to come to the bedside of a deceased or dying loved one.
“Sarah: What is the best part of your job? What is the worst part?
Christine: The best part is being able to ease suffering. The worst part is when I can’t.”
In early March I could see a tidal wave coming--we were starting to understand just what had happened in northern Italy and watching our PPE supply eviscerate and wide swaths of staff taken off work due to sickness and possible exposures--it was scary. I really geared myself up as a support for loved ones and staff. Patients suffering from COVID were often too sick to meaningfully participate in an assessment, and we were trying to limit transmission by limiting contact with non-clinical staff. I was seeing signs of acute traumatic stress within myself and my colleagues. There was very little chatting between staff that are usually jovial and warm. Their phones buzzing as family members panicked, asking them not to come to work, and some staff began making plans to move out of their own homes. Back then, visitors were permitted, but limited, and the department was eerily quiet. When loved ones would cry at the bedside, the sound would echo, and with it traveled fear and trauma. Many staff had sore and torn skin from PPE and make-shift PPE. The group dynamics, along with some physical markings, contributed to a mentality and culture shift from healthcare to conflict zone.
My role as a mental health provider began to absorb some of the responsibilities of a Chaplain. Patients and families expressed tremendous spiritual distress and would frequently request prayer at the bedside and over the phone during a clinical assessment.
Sarah: What have been some of your most important tasks/interventions during the pandemic?
Christine: I continue to feel that my most important intervention is a thorough initial assessment. The critical components of that assessment are vital during a pandemic, a part of that assessment is establishing a surrogate decision maker or receiving a copy of an Advance Directive or POLST. Sadly, the COVID deaths I have seen in the ER have been a rapid decline, so establishing this information is definitely a time-sensitive priority.
During an assessment, I’m basically formulating a genogram in my mind, trying to get a sense of care available to the patient. For patients who have COVID, the news of that positive test presents an immediate crisis--families wonder if they can safely reside together and what arrangements to make. I try to walk them through next steps and what to expect over the next few weeks, and direct them to COVID information and resources for testing etc.
I am encountering significant mental suffering, emotional anguish and considerable spiritual distress among patients and their loved ones. The trauma of losing a loved one to COVID is cruel and the ripple effects are vast. For example, I had a patient who tested positive for COVID. She was tearful and terrified, reporting to me her pastor had just died of COVID. This care setting offers spiritual care for any patient by phone or in person. I like to utilize the FICA assessment developed by Dr. Christina Puchalski at George Washington University. I often uncover important goals of care during the FICA discussion.
Sarah: How has wearing a mask all day changed your interaction with patients?
Christine: Clinical practice is so very different when I am wearing an N95 all day--every patient is in a mask. My voice is muffled, so I am very deliberate with my intonation and have developed a much more sing-song inflection since they cannot see me smile. I have started to wear different eye makeup since my eyes are my only visible way to emote. My impression is that patients are reassured seeing clinical staff who appear well groomed under all their PPE--it seems just a little more normal. Like being on a plane during turbulence, but the flight attendants are calm and put together.
Sarah: What is the policy at your hospital on visitors? How has it affected patients and staff?
Christine: At this time, the hospital allows no visitors at all. Patients and loved ones suffer greatly. The staff are spending huge emotional energy to be present at the bedside in more meaningful ways. I’m trying to be more vigilant of comfort items and call lights to diminish medical trauma. Today I stood at the bedside holding the hand of an elderly woman during her bedside procedure. I let her grip my right hand and with my left hand I stroked her hair and spoke softly to her. This is what we do now. It is clinically necessary to care for her not just as a patient but as though she is my own mother since her bedside is empty. This human contact appears to greatly diminish her fear and help manage her pain.
I’m also notified by clinical staff when they encounter family who are inconsolable over the phone and have concerns the loved one lacks adequate emotional care. The dynamic among staff in my department appears to be incredibly positive. The shared disposition is becoming lighter since those early days. Easier laughs and more natural interaction. This current of positivity carries us through tragedies and suffering and helps combat compassion fatigue.
Sarah: Did you ever become sick?
Christine: Yes. March 16th was the last day I worked before my family and I became sick with what we presume to be COVID. At that time, there were no tests available, and we were told to remain at home. We were fortunate to manage our symptoms at home, but it was a scary time. I kept in touch with colleagues by text, as we were among the first to become sick. I wanted to be open with them about what we were going through, since we both knew they would be next. This transitioned our relationship from friendly/professional into a tight bond.
Sarah: How did it feel coming back to work?
Christine: Returning to work after recovering was a relief but I was torn. I have three young children, at that time they were ages 8 months to 4 years. My training and experience drew me to come back; I was eager to be useful in a crisis. However, I was very worried my children would suffer because of my job. I sought out strategies to limit infection transmission returning to our home by having good disinfectant routines. Ultimately there was work to be done and I wanted to do it.
I wanted to lead by example for my colleagues, strengthening their hope and resolve by returning to work after sickness. As a mother with young children, my return to work was a strong statement because there was so much to fear because still so much is unknown. I relished the hope and encouragement I could give when colleagues would ask me about our experience of sickness. I could see my story and others like it build resiliency among colleagues as we each attempted to develop a new understanding of the value and risk of our work.
Having lived through chest pain, shortness of breath and painful neuropathy, I experienced the fear first hand and saw the value of psychological support and mental health care. My husband and I guided each other through breathing exercises, shared our fears and employed a dark humor. We were vigilant and responsive to symptoms, kept in touch with our doctor--but worked hard to stay connected and find humor throughout the day. Humor carried us through so much. It seemed to be the only anecdote to fear.
Usually these lessons would be considered personal or anecdotal. But in a crisis, it becomes necessary to maintain mental buoyancy among a team. Many households experience stressors of all kinds during this time. I find clinical value in some self-disclosure to colleagues. I am careful not to provide medical advice to families, but I am happy to share with a fellow parent that my children have been sick too. We are bonded strangers in those moments and I watch as their eyebrows gradually unfurrow, their posture starts to relax. There are usually tears, but they are tears of release, connection, and hope. I cannot offer reassurance, but I can offer connection.
“My role as a mental health provider began to absorb some of the responsibilities of a Chaplain. Patients and families expressed tremendous spiritual distress and would frequently request prayer at the bedside and over the phone during a clinical assessment.”
Sarah: What are some of your greatest concerns/worries on the job now?
Christine: In the early days I saw this COVID tsunami coming for communities of color – typically they are the first and most hard hit economically and have the least access to preventative healthcare, more pre-existing conditions, and fewest resources. I lamented in prayer and cursed in anger with my colleagues for the coming onslaught these communities would face. During moments I have allowed myself to consider it deeply, and I’m angry and broken-hearted.
I have many worries, but I’ll outline 5 for now:
1) Loved ones are not yet being contacted in real time for contact tracing and consultation due to lack of infrastructure. I wish I was seeing that resource and information ramp up faster. Our local services are amazing, but the lack of federal guidance is a daily hindrance.
2) The vast and deep suffering of patients and loved ones who cannot be together in the hospital. The COVID-19 deaths I have seen have been too rapid for family to reach the bedside prior to death. The patient can be relatively stable and then crash. Knowing a loved one died without family is a tremendous pain that cannot be described or quantified. The impact of which will be felt exponentially and throughout generations.
3) I’m worried by the patients I’m not seeing. Folks who need their routine medical care and important surgeries, victims of crime who are not seeking services or medical care, victims of intimate partner violence who are staying at home. It’s terrible knowing the next waves of this virus will be depression and desperation – exacerbating stressors for every form of suffering.
4) It’s also hard to see that some politicians and sectors of the public seem to be (messaging) healthcare as the enemy of the economy and freedom. I’m very upset by protest images of nurses standing in front of an angry public, many of whom will come through our doors for help. I’m worried about people’s search for answers and finding solace in conspiracies. I’m worried when I hear people say their life-long relationships are breaking down because of online arguments. I see folks lacking the ability to distinguish science from opinion, politics from public health. It’s a helpless feeling. Some folks don’t understand that without a shutdown, at least in this area, it would have been a slaughter. In this area we avoided that level of a crisis--we got ahead of it--for now. I’m worried for the gullible folks who are taking part in a false premise of freedom vs tyranny, who observe mask wearing as a rights infringement. I’m young, I’m healthy--you better believe I wear a mask to protect others. With COVID, our own breath is effectively second-hand smoke. Angrily refusing to wear a mask is like blowing smoke into someone’s face--but worse.
5) The economic and emotional damage is coming at us like an avalanche. Although our kids are breathing cleaner air these days, their national debt load will be so much higher than my lifetime and economic disparity will widen. I’m worried for the desperation that economic hardship will bring. I’m worried for the millions of children who are sheltering in abusive homes and cannot go to school for relief. I’m worried about partners in abusive relationships, feeling even more trapped. I’m worried that perpetrators will be increasingly abusive because of stress and their victim’s complete social isolation. I’m worried for elders who live alone and will suffer a fall, and that neighbor who usually walks by may not hear them calling for help. I’m worried for my own safety, that someone may assault me as a healthcare worker--a symbol for many of economic devastation and rights infringement.
Sarah: What is the best part of your job? What is the worst part?
Christine: The best part is being able to ease suffering. The worst part is when I can’t.
Sarah: How do you separate your personal life from work?
Christine: It’s not hard to separate my personal life from my work. After 7 years of this, I’m a well-oiled HIPAA machine and don’t talk about work at home. But it is harder to separate my work from my personal life. When I see friends and family putting up questionable information online, making light of the virus, or inciting arguments about how they are ‘against’ social distancing etc…it’s hard not to take it personally. In those discussions it feels like I am on the receiving end of so much misplaced anger. Healthcare workers did not create the COVID-19 crisis. We do not have job security. We risk our lives and those of our families because we believe it is right. We are prepared to work and called to serve. But increasingly I feel this false narrative being developed that healthcare workers are standing in the way of economic recovery. It feels supremely dangerous and unfair.
Sarah: Are you able to find hope in the midst of so much uncertainty?
Christine: Absolutely!
Sarah: As restrictions in LA County change, what can people do to help healthcare workers like you?
Christine: This is a great question. I think it comes down to patience, education and generosity. Be patient with our public health officials--a novel virus is a maniac to understand, let alone predict. Continue to educate yourself and your loved about ways you can limit transmission at every stage of activity i.e. at home, work, school etc. Lastly be generous. Donate to food banks, and if you own a business, donate food to a local hospital or nursing home. Send in PPE, posters, cards, flowers--anything and everything that will encourage workers. Appreciation and encouragement builds resiliency in the souls and immune systems of essential workers.
Sarah: Thank you, Christine!
Christine Chester, MSW, LCSW, works in the Los Angeles area as an Emergency Room Social Worker.
Sarah Butcher, LMFT, specializes in treating children, teens, new and postpartum parents, and young adults. Her work with children in developmental play therapy led to her certification as a DIR Intermediate Floortime provider.